Principal Care Management (PCM) Services: Specialized Care for Single High-Risk Conditions
Optimized Revenue and Clinical Excellence for Specialized Chronic Conditions
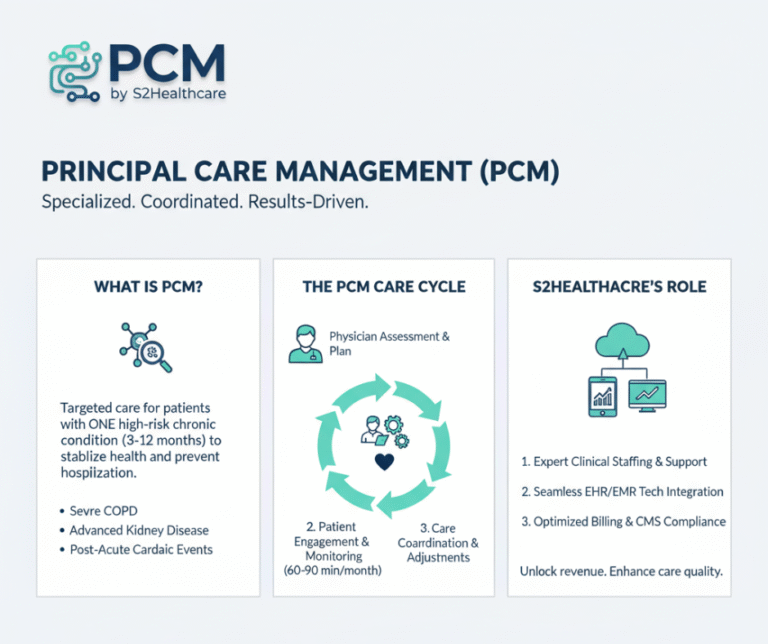
In the shift to value-based care, the single, high-complexity patient cannot be overlooked. S2Healthcare delivers a robust, turn-key Principal Care Management PCM solution, guaranteeing rigorous clinical oversight, meticulous CMS compliance, and the successful capture of specialized Medicare reimbursement that your dedicated care efforts deserve.


Foundational Deep Dive: Understanding the PCM Mandate
PCM is not merely an extension of Chronic Care Management (CCM); it is a distinct, intensive care model established by the Centers for Medicare & Medicaid Services (CMS) specifically for patients with a single, severe chronic condition. This condition must be reasonably expected to last between 3 to 12 months, or until the specific treatment goals are achieved. This targeted scope allows for a deeper dive into one diagnosis, which is particularly vital for specialty practices (e.g., Cardiology, Pulmonology, Nephrology) and Primary Care Providers managing acutely unstable cases.
| Clinical Expertise & Patient Engagement | Technical Integration and Financial Compliance |
| Dedicated, Extended Clinical Team | Seamless EHR Integration & Audit Security |
| Our model provides certified, dedicated clinical staff who act as a direct extension of your practice. They operate under your specific protocols and physician oversight, ensuring continuity and clinical integrity across the PCM service line. | We utilize a proprietary, HIPAA-compliant platform designed for the complexities of chronic care management. Our system achieves bi-directional data flow with all major EHR/EMR systems (e.g., Epic, Cerner, Athena). |
| Key Deliverables: | Key Deliverables: |
| * Required Time Met: Reliably perform and document the mandated 60-90 minutes of interactive care per patient per month, focusing on condition stabilization. | * Automated Audit Trails: Every touchpoint, communication, and care plan revision is automatically logged and time-stamped, providing 100% audit-proof documentation required by CMS. |
| * Care Plan Oversight: Meticulous review and proactive revision of the disease-specific care plan, including tracking adherence to treatment goals and risk factors. | * Real-Time Data Visualization: Provides your clinicians with immediate, comprehensive patient care dashboards showing progress, goal attainment, and risk stratification for quick, informed review. |
| * Specialty Coordination: Serve as the central hub for communication, ensuring seamless transitions and timely information exchange between the patient and other specialists (labs, rehab, etc.). | * Error-Free Billing: We manage the complex CPT code submissions (G0296, G0297) and ensure all service minute thresholds and consent requirements are reliably met, maximizing claim acceptance and monthly recurring revenue (MRR). |
Financial Certainty: Maximizing PCM Reimbursement
Precision Billing for PCM CPT Codes
Maximizing reimbursement begins with precision in coding. Principal Care Management utilizes specialized CPT codes, including G0296 (Clinical Staff Time) and G0297 (Physician/NPP Time). S2Healthcare’s robust process guarantees the accurate capture of all billable time and services, ensuring the complex service requirements—such as meeting the 60-90 minute monthly threshold and documenting patient consent—are flawlessly met. This meticulous attention to detail minimizes claim denials and secures a consistent, dependable monthly recurring revenue (MRR) stream for your practice.
Mitigating Documentation and Audit Risk
In the realm of Medicare reimbursement, documentation is your greatest defense. Our platform provides automated, time-stamped audit trails for every care interaction. This eliminates the compliance risk inherent in manual tracking, proving conclusively that the required clinical services were delivered and coordinated under the billing provider’s direction. By adhering to the strictest CMS audit standards, S2Healthcare provides the financial certainty your practice needs to invest confidently in this specialized care model without fear of recoupment.
Converting Clinical Effort to Guaranteed Profit
Principal Care Management fundamentally changes the financial model by converting previously uncompensated non-face-to-face clinical effort into a robust profit center. Instead of care coordination being a cost burden on your practice, our managed service ensures you are fully reimbursed for the intensive, life-saving work your team performs for single high-risk patients. This strategic shift in revenue capture supports better resource allocation and fuels the expansion of quality care services across your entire patient population.
A Strategic Edge in a Quality-Driven Landscape

Successful PCM implementation does more than generate revenue; it strategically positions your practice for success in a healthcare environment increasingly focused on quality and value metrics.
Elevated MIPS Performance:
Active participation and demonstrated outcomes in programs like PCM contribute positively to your quality and improvement activity categories within MIPS, driving a higher final score and maximizing incentive payments.
