MACRA/MIPS Framework for the Future of Healthcare
What is MACRA? The Foundation of Value-Based Care
Tired of MIPS feeling like a punitive administrative burden? At s2healthcare.us, we don’t just ensure compliance; we transform MACRA’s complexity into a predictable revenue strategy. Our specialized MIPS services, powered by strategic integration of Remote Patient Monitoring (RPM) and Chronic Care Management (CCM), are engineered to do more than just avoid penalties. We proactively optimize every performance category—Quality, Cost, PI, and Improvement Activities—guaranteeing you the highest possible MIPS Final Score. This focus not only secures the maximum positive payment adjustment for your practice but also enhances patient health outcomes, creating a seamless, profitable alignment between regulatory requirements and superior care delivery. Partner with us to stop worrying about penalties and start earning the MIPS bonus you deserve.
Merit-based Incentive Payment System (MIPS)
This is the track most providers currently participate in. It consolidates and replaces previous programs (PQRS, EHR Incentive Program, and Value-Based Payment Modifier) into one streamlined performance-based payment system.
Advanced Alternative Payment Models (Advanced APMs)
These are payment models where providers take on more risk for patient outcomes in exchange for higher potential rewards.
The Four Performance Categories of MIPS
| Category | Weight (Typical) | Focus | Compliance Strategy |
| 1. Quality | $30-40\%$ | Reporting on quality measures that demonstrate the delivery of high-value care (e.g., preventative screenings, chronic disease management). | Select and report on 6 measures, including an outcome measure. |
| 2. Improvement Activities (IA) | $15\%$ | Engaging in activities that improve clinical practice, patient engagement, and care coordination. | Perform 2-4 activities for a minimum of 90 continuous days. $\rightarrow$ This category is an ideal fit for CCM and RPM services. |
| 3. Promoting Interoperability (PI) | $25-30\%$ | Using certified Electronic Health Record (EHR) technology to exchange health information and engage patients. | Report on required measures concerning e-prescribing, health information exchange, and patient access. |
| 4. Cost | $10-30\%$ | Assessing the total cost of care and resource utilization relative to patients served. | Calculated by CMS based on Medicare claims data. No direct reporting required. |
Avoid Penalties & Join S2healthcare.us now
Avoid MIPS penalties and maximize your Medicare reimbursement. The Merit-based Incentive Payment System (MIPS) is complex and constantly changing, but your focus should remain on patient care. Book your free, 15-minute MIPS Consultation with s2healthcare.us today. We will review your practice’s MIPS eligibility, analyze your current performance data, and outline a clear strategy to ensure guaranteed compliance and a maximum positive payment adjustment. Schedule your consultation now to simplify MACRA and secure your financial success.


Critical MIPS Compliance Requirements and Deadlines
Staying ahead of the regulatory timeline is non-negotiable for successful MIPS participation.
- Eligibility: MIPS applies to most Medicare Part B providers who meet the low-volume threshold (based on Medicare billing and patient counts).
- Performance Period: The reporting period for most MIPS categories is the full calendar year (January 1 – December 31). Improvement Activities and Promoting Interoperability have a minimum 90-day reporting period.
- Submission Deadline: Data submission typically runs from January 1 to late March following the performance year.
Why Choose S2Healthcare.us for MIPS/MACRA Compliance?
We don’t just help you comply; we help you succeed. Our approach is built on expertise, technology, and a commitment to your financial health.
- Expert Authority: Our team consists of certified compliance experts who live and breathe MIPS and MACRA.
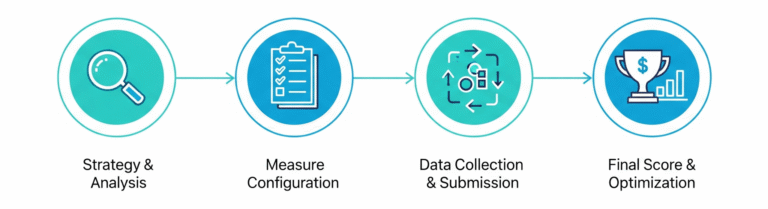
- Full-Service Partnership: We provide end-to-end support, from eligibility checks and strategy development to full data submission.
- Proven Results: Practices working with us consistently outperform the national average MIPS score.
- Integrated Solutions: Access to our premium RPM and CCM services that are strategically aligned with MIPS requirements.
Our MIPS/MACRA Service Offerings Include:
- MIPS Eligibility Check and Participation Strategy
- Performance Category Optimization Consulting
- Quality Measure Selection and Benchmarking
- Full Data Aggregation and Submission
- Penalty Mitigation and Appeals Support